Specialty access barriers: How technology can help
2020 was a difficult year for many patients, but new data may signal a brighter future ahead
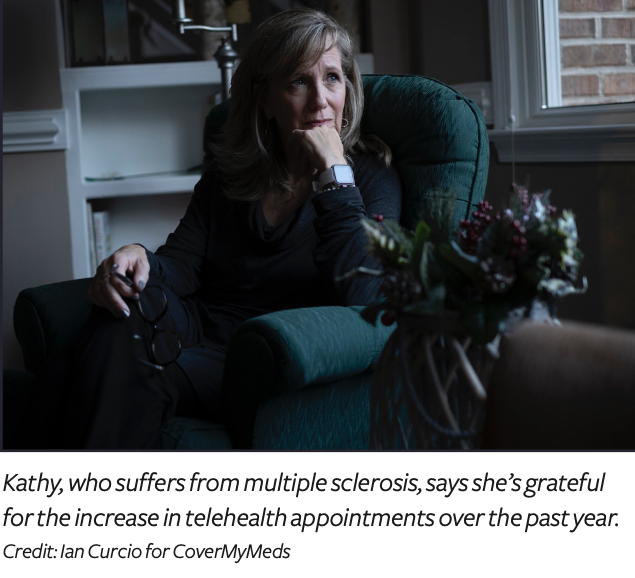
Affording the high cost of specialty medications can feel insurmountable for many patients. For others, simply accessing their prescribed therapy can prove daunting. For example, take Kathy *, a patient featured in the 2021 Medication Access Report. Kathy juggles treatment plans and test results to manage her multiple sclerosis (MS)—a process she described as stressful and detrimental to her health. Some days, she’s left with a momentary loss of mental clarity, or “cognitive fog.” “It’s too much to ask a patient to have to do, and it’s affected my health, no question,” Kathy said.
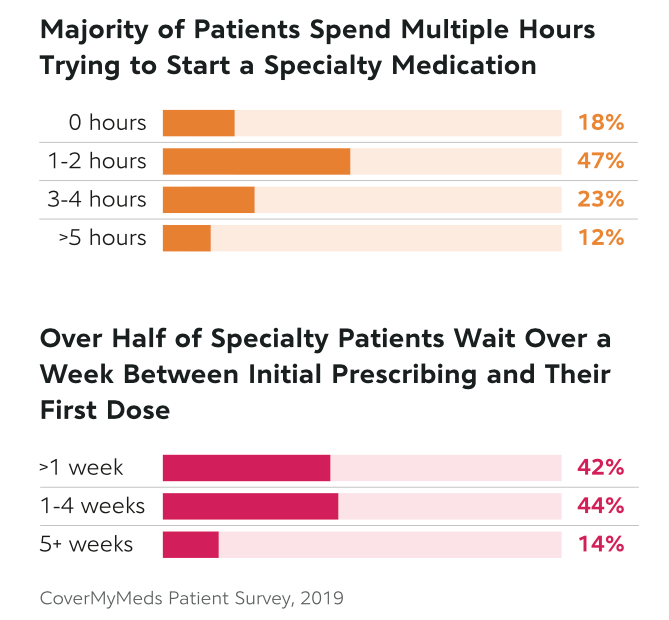
Specialty patients surveyed to inform the 2021 Medication Access Report shared similar access challenges. Eighty-two percent of those prescribed specialty therapies reported spending an hour on the phone coordinating care to begin their therapy. Over a third spent at least three hours.1 Medication access and adherence challenges can be so significant for specialty patients, up to 27% of prescriptions and therapies are abandoned—or never started at all.2
Historically, support services have been available to help patients with these obstacles. But traditional hub programs and specialty patient workflows have faced significant hurdles over the years. Their impact tends to be dampened by low awareness, minimal connectivity and manual workflows.
And since traditional, manual workflows rely on outdated, less immediate forms of communication—including phone and fax—they often leave providers in the dark about the patient journey once they’ve prescribed therapy or enrolled their patient into the manufacturer-sponsored patient services. These inefficiencies can result in treatment delays of up to eight weeks.3 In the interim, patients have reported deteriorating health and worsening of symptoms.4
But it’s not all bleak news. Progress is here. Social distancing measures sparked by the Covid-19 pandemic might have cleared long-standing access obstacles for specialty patients. Among them: eased restrictions which enable some patients to take their therapies at home and tech-enabled patient support services that electronically connect the healthcare network to clear access hurdles for specialty patients. These solutions were already primed for widespread use, but the Covid-19 pandemic is helping achieve widespread adoption.
How Covid-19 uncovered and helped solve unique access challenges
In the 2021 Medication Access Report, we investigated the unique access challenges specialty patients experienced due to Covid-19. For one, patients with preexisting conditions—such as chronic and rare diseases—faced a higher risk of contracting Covid-19. This risk made any in-person interactions to access their needed medications (such as a doctor’s visit) potentially life-threatening.
Further complications arose when the condition required a specialty medication, which are often administered non-orally or require diagnostic testing prior to use. Importantly, a medicine’s method of administration can influence where patients receive therapy. Some may be able to stay home, while others may need to go to a provider’s office or outpatient facility with clinical staff on standby.5
When Covid-19 prompted social-distancing measures, the use of key autoimmune, oncology and osteoporosis drugs fell by as much as 53% below 2019 levels.6 Data from the 2021 Medication Access Report point to reasons why we may have seen such a decline in utilization. Nearly half of providers said they changed how they approached specialty patient appointments due to Covid-19. Nearly one in five said they saw a decrease in patient therapy compliance.7
Kathy was among those who stayed away from medical facilities used by providers to administer specialty therapies like infusion and injectable drugs.8 (“I’m scared to go any place,” she said.) When her neurologist ordered routine blood work, Kathy asked if they could use results from a previous visit.
For the same reason, Kathy said she’s grateful for the increase in telehealth appointments over the past year. Even after the initial Covid-19 spike in spring 2020, telehealth use stayed exponentially higher than ever—over 2,000% over baseline levels through the end of 2020—suggesting a more permanent option for provider access.9
In other words, the therapies patients were prescribed before the Covid-19 pandemic became easier to access because of a shift toward remote-capable technology solutions. What’s more, patient support services driven by technology have contributed to a 34% reduction in time to therapy.10
But even though the Covid-19 pandemic disrupted specialty medication prescribing, distribution and administration, the shifts to keep patients out of healthcare facilities may have paved the way for more accessible therapies.
When many payers eased restrictions on home infusions to allow specialty patients improved access to their medications,11 patients followed their lead.12 Data shows many patients who received provider-administered drugs in hospitals or healthcare facilities shifted to self-administered oral, patient-injectable or home infusion drugs.13 While in-person treatments are currently below baseline levels, remote treatments are up by nearly 600% over baseline levels, now accounting for over 20% of specialty treatments.14
Many providers also saw improved quality of care and patient satisfaction in these moves.15 After all, home administration means patients don’t have to miss as much work, reduce time spent in waiting areas and even learn more about their own condition and medications as they become further integrated in their own care.
These trends show promise for the future.
What’s next? Keep the momentum going
Tech-enabled hubs were developed to help patients navigate the process of starting and maintaining complex therapies, but other stakeholders stand to benefit from this electronically connected healthcare network, too.
These models connect an established and engaged healthcare network—from providers to payers to pharmacists to life sciences—via a single platform. Through these innovative services, providers can electronically navigate affordability, pharmacy access and clinical support—and have real-time visibility into the status of each step.
Ideal tech-driven patient support programs allow providers to electronically enroll patients into support services designed to provide financial assistance, benefit coordination, pre-therapy support, necessary lab work and managing adherence programs in one, centralized place.
Such technology also allows for automatic prior authorization (PA) determinations based on preset payer-defined criteria. The opportunity for real-time responses can accelerate provider decision-making and limit unnecessary treatment delays for patients. Most importantly, these programs meet the provider within their current workflow and create immediate awareness of patient assistance support. This helps solve access challenges for providers and the patients they serve.
To keep this momentum going, lessons can be drawn from other healthcare advancements driven by innovative technology. Through our work automating the PA process, we found that disjointed processes can be streamlined through connectivity, but for these advancements to be meaningful to patients, provider adoption was critical. It’s heartening knowing what we’ve learned about how technology has advanced patient support services as well.
Finally, we must not forget about the person at the other end of the computer screen. Patients build trust and confidence in providers and their treatment plans through personal interactions with their clinical and care teams.
The ideal technological solutions don’t ignore these interactions but instead embrace them. By connecting all the stakeholders working for the patient—from the field team to case managers—tech-enabled patient support services that connect the healthcare network make sure everyone has a real-time view of the patient. This synchronicity also means all stakeholders can work together to support the patient without duplicating work.
For the patient, these experiences can build trust and confidence, which are particularly important factors in clinical and care coordination. And though more work remains, these moves are encouraging and show us a path forward—raising awareness of the positive impact of tech-enabled patient support services and continuing to push forward innovation within the specialty workflow.
The work is worth it. The impact potential is real.
About the author

Erica Conroy, PhD, VP of Specialty Business, CoverMyMeds
* The patient’s last name has been omitted to protect their privacy.
References
1. CoverMyMeds Patient Survey, 2019
2. IQVIA Medicine Use and Spending in the US: A Review of 2016 and Outlook to 2021
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6234348/?report=classic
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6234348/?report=classic
5. https://www1.magellanrx.com/documents/2019/03/medical-pharmacy-trend-report_2018.pdf/
6. Monitoring the Impact of COVID-19 on the Pharmaceutical Market, IQVIA, 2020
7. CoverMyMeds Provider Survey, 2020
8. Specialty Pharmacy Keeps Disrupting Buy-and-Bill—and COVID-19 Will Accelerate It, Drug Channels, 2020
10. CoverMyMeds Data on file, 2020
11. “New Federal Rule Could Affect Infusion Site of Care Amid COVID-19 Pandemic,” Avalere, 2020
12. “Monitoring the Impact of COVID-19 on the Pharmaceutical Market,” IQVIA, 2020
13. “Monitoring the Impact of COVID-19 on the Pharmaceutical Market,” IQVIA, 2020
14. “Monitoring the Impact of COVID-19 on the Pharmaceutical Market,” IQVIA, 2020
15. “Home Infusions and Home-Based Chemo: The Innovation of Penn Cancer Care at Home,” Penn Medicine, 2020