Read time: 5 minutes
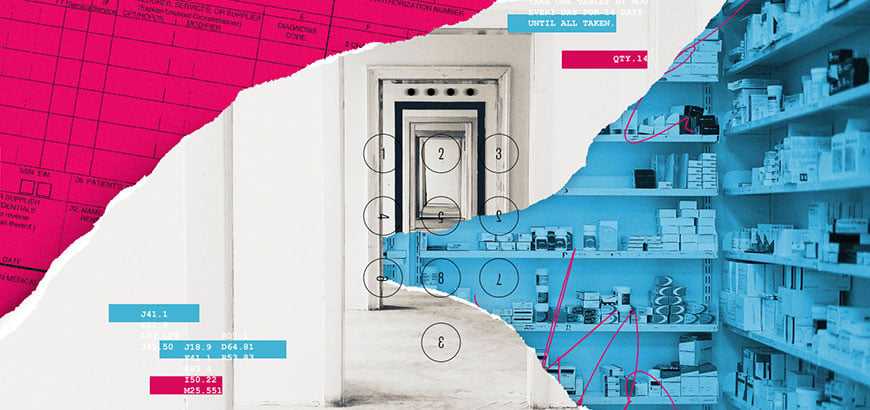
In 2019, 4.22 billion Rx prescriptions were filled in the U.S. From a historical perspective, most people think that getting a prescription filled simply involves a consultation with a doctor and a trip to the local pharmacy. In reality, it’s a multi-step and often complex process involving several players and numerous technologies.
As a major healthcare technology solutions provider, part of McKesson’s job is to create and offer a variety of systems and mechanisms to equip care providers, insurance companies and pharmacists with clinical and financial information that help connect patients to affordable and accessible medical treatments.
Here are five of the many examples of the behind-the-scenes technologies from McKesson that ultimately can help improve overall health outcomes.
1. Navigating prior authorization
Just because a drug is available and effective for a patient’s specific condition doesn’t mean the patient will automatically have access to it under his or her insurance coverage. One of the most common hurdles for a patient who needs a specific medicine is the process of prior authorization (PA). A PA request essentially is a “permission slip” from the patient’s health insurer indicating that they agree to cover the cost of a medication after the insurer determines that it’s the most appropriate and cost-effective therapy for the patient’s medical condition. Traditionally, the PA process was paper-based and required pharmacists, providers and health plans to exchange a series of phone calls and faxes that could take days—often delaying therapy for the patient.
Technologies like those from CoverMyMeds simplify the PA process by making it fully electronic, which ultimately leads to faster determinations and medication availability.
For patients with complex and chronic specialty diseases, the process of gaining streamlined access to specialty therapies can be especially cumbersome. New hub solutions like AMP: Access for More PatientsTM, a collaborative effort between CoverMyMeds and RxCrossroads, improve patient access to specialty medications.
2. Ensuring specialty drugs are handled with care
Specialty drugs are made for rare diseases and other complex illnesses. They can be inhalable, injectable, infusible or oral. Some are unique to a patient, such as CAR T-cell therapy, a treatment often used for certain cancers that is made using a patient’s own blood cells.
Patients depend on getting these specialty medications quickly, but they can’t usually buy them at retail pharmacies. That’s because specialty drugs tend to be fragile, have short shelf lives, and can require maintaining a specific temperature. Moisture, light, heat and movement can all reduce their potency.
Specialty drug distribution technology helps to maintain the safety and efficacy of specialty drugs while they are being transported. The technology helps to keep them in precise conditions by using sensors that actively monitor the drug environment to maintain safety and efficacy, as well as navigation technology that ensures the timeliest routes for delivery.
Drugs that are destined for specialty practices also need to be accounted for from the time they arrive at the clinic until they are dispensed. Inventory management solutions, like McKesson’s Lynx®, help to ensure that high-cost drugs are secure for authorized access only and that the right medication is delivered to the right patient at the right time.
3. Breaking down affordability barriers
 According to a 2019 survey by the Kaiser Family Foundation, 24% of people taking prescription drugs responded they had difficulty affording them.
According to a 2019 survey by the Kaiser Family Foundation, 24% of people taking prescription drugs responded they had difficulty affording them.
The good news is that technology can help address affordability issues at the point of prescribing. When a doctor selects the intended medication, services from McKesson like RelayHealth and CoverMyMeds are able to quickly determine the price of the prescription at the patient’s preferred pharmacy and the drug’s out-of-pocket cost, assist prescribers in determining whether clinically appropriate alternatives may have a lower cost for the patient, indicate whether the patient qualifies for financial assistance, and specify if there are any PA requirements. If a PA is required, the technology is equipped with functionality to proactively initiate a PA request. With a few taps, technology can knock down financial barriers that can keep a patient from walking out of a pharmacy without the medications they need.
The high cost of specialty drugs, particularly oncology treatments, are another aspect of healthcare that is significantly affecting patient financial challenges. One tool, Clear Value PlusSM, not only supports the PA process, but also helps oncologists identify and compare appropriate evidence-based treatments that are covered by the patient’s insurance policy and also offers lower out-of-pocket costs to the patient.
4. Giving patients the power to choose
Prices for medications can vary from one pharmacy to another, which can be difficult to evaluate – and that’s before taking into account the terms and conditions of a particular health insurance plan. Consumer-facing platforms like ScriptHero Marketplace let patients compare prices of prescriptions for free and in real-time, and help them decide where they get it filled and how they want to pay for it. In many cases, patients can often pay less in out-of-pocket costs if they pay with cash instead of using their health insurance benefits.
5. Achieving medication adherence
According to a review in the Annals of Internal Medicine, 20% to 30% of prescriptions are never filled, and about half of medications for chronic disease aren’t taken as prescribed. That could mean the patient doesn’t finish the full course, doesn’t follow the dosing instructions, or doesn’t take the full course of therapy. This all results in sub-optimal outcomes for patients.
While cost is one reason a patient might not pick up a prescription or continue on therapy after the initial treatment, there are also other barriers. These can include not understanding what a drug is for, a lack of transportation to the pharmacy, a dislike of the drug’s side effects and even plain forgetfulness. Adherence technology from McKesson Pharmacy Systems can help. It tells pharmacists if patients have picked up their prescription and subsequent refills. If they haven’t, the pharmacy can remind them by phone or text message, or counsel them to be sure they understand what condition the drug treats and its possible side effects.
Although the value of these technologies is delivered in the background of healthcare, it’s important to recognize that people every day are creating innovations that power our healthcare system that improve the quality of life for everyone. And that’s certainly something to know about.



Share
Post
Post
Email